Hypoplastic and Hypomineralised Teeth
The term "hypoplastic" means less quantity of enamel, and the term "hypomineralised" means less mineralised tissue. Basically this involves a tooth which is less mineralised therefore more porous. A hypoplastic tooth has reduced amount of enamel so the surface may be rough. Your child may have teeth which have developed in this manner. The most common teeth to be affected are the second primary molars which erupt at the age of 2 1⁄2 years or in the permanent dentition the first permanent molars which erupt at age 6.
Hypoplastic and hypomineralised teeth develop as a result of an event which has occurred during the development of the enamel. There have been over 100+ different sources identified in causing hypoplastic and hypocalcified teeth. Some of these causes include infections (tonsillitis, chest infections, ear infections, acute gastrointestinal infections etc), fevers, convulsions, nutritional imbalances, electrolyte imbalances, measles, chicken pox, hand, foot and mouth diseases, other viral infections, etc, etc.
In some children when these infections or causes occur, the cells which lay down the enamel start to lay down enamel which is less mineralised and more porous therefore giving the appearance of mottled, yellow or white opacities, or the enamel is laid down in very thin sheets. These areas are more prone to breaking and wearing down and rough surfaces will attract plaque and food retention. Ultimately these teeth can become prone to developing decay.
The severity of hypoplasia and hypocalcified teeth varies where some children will have very slight yellow/white flecks and no discomfort, ranging right through to where the entire tooth surface may be affected and the child experiences sensitivity to air and cold substances. The management of these teeth depends on the severity. Each child is different and in mild cases fissure sealants to protect the surfaces on top of the teeth can be applied or restorations. Where over 50% of the surface is involved a crown (stainless steel) may be required to protect the surface until the child is old enough to have a permanent gold or ceramic crown.
In more severe cases a consultation with an orthodontist may be required and a decision to extract the severely affected teeth may be taken. This would allow the developing second permanent molars to take their place. An OPG radiograph is taken by the orthodontist which will show all the new developing permanent teeth and their position. The reason for taking out these severely affected teeth in children is to avoid them from having repetitive dental care (restorations, root canals, crowns) over time on these same weak teeth. If these weak teeth are extracted while the children are growing there is a good chance that the second permanent molars which are developing in the bone behind these affected teeth will drift forward and erupt into their spaces.
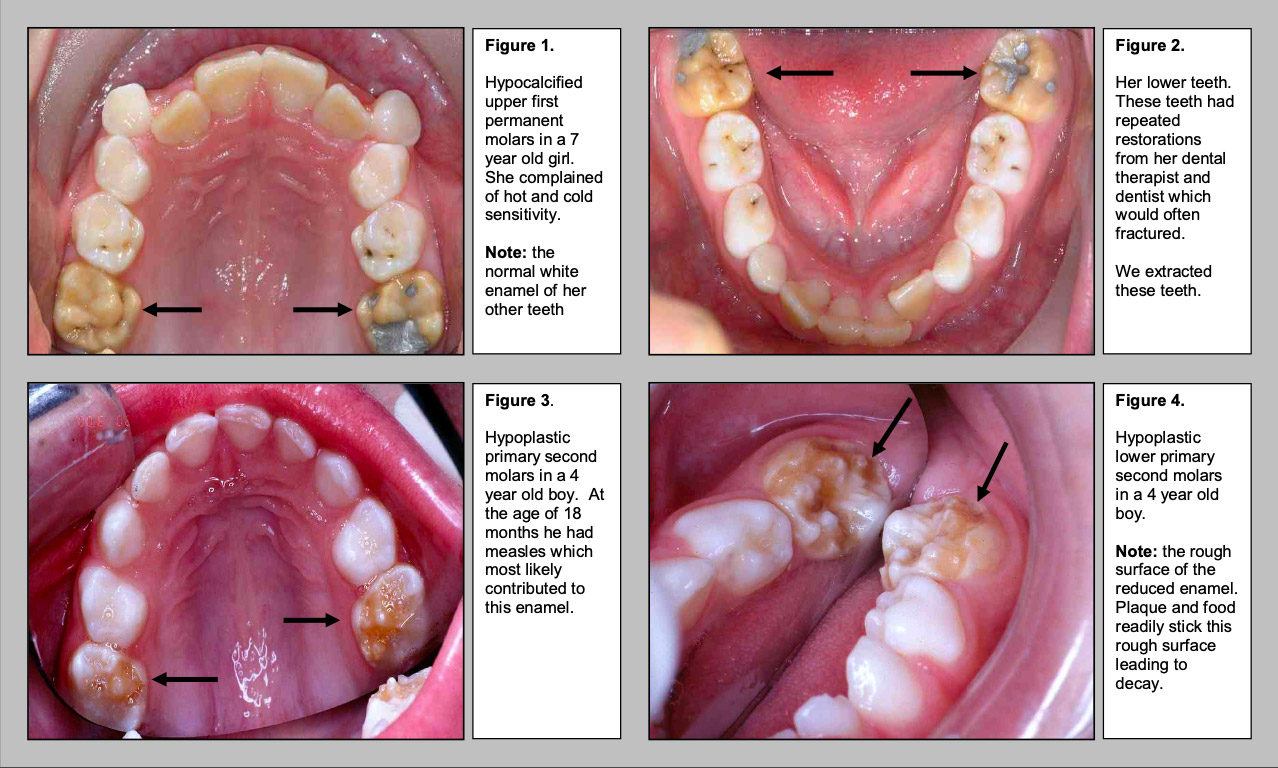
Figures 1 and 2 show hypomineralised permanent molar teeth for a seven year old girl. The teeth have a yellow color in comparison to her remaining teeth which have white enamel. When drilling into this affected enamel it is similar to drilling into cheese. This hypomineralised enamel is very porous and fissure sealants and fillings do not bond well to it. She experienced multiple restorations from her dental therapist and dentist, which continued to break and fail. An OPG radiograph showed the presence of permanent second molars developing in the bone, so it was decided to extract the affected teeth under a short general anesthetic and allow the second permanent molars to drift forward.
Figures 3 and 4 show hypoplastic second primary molars in a 4 year old boy. The surface is rough, allowing plaque and food to trap readily onto this surface leading to decay. Stainless steel crowns were placed on these teeth.
